Bacterial Pathogens Priority List Updated by WHO
Antibiotic resistance is a major public health problem around the world. It happens when bacteria become resistant to medicines, making infections hard to treat. The World Health Organization (WHO) recently changed the Bacterial Priority Pathogens List (BPPL). This is an important step that shows they are serious about solving the problem. The goal of the revision is to put bacteria that are the biggest threats at the top of the list and help researchers come up with successful new antibiotics.
What is Bacterial Priority Pathogens List (BPPL)?
The BPPL sorts germs that are resistant to antibiotics into groups that help research and development (R&D) focus on making treatments that work. Its goal is to focus resources on fighting the most dangerous bacteria in the best way possible. WHO wants to stop the spread and effects of antibiotic resistance (AMR) around the world by keeping this list up to date.
Importance of the BPPL Update
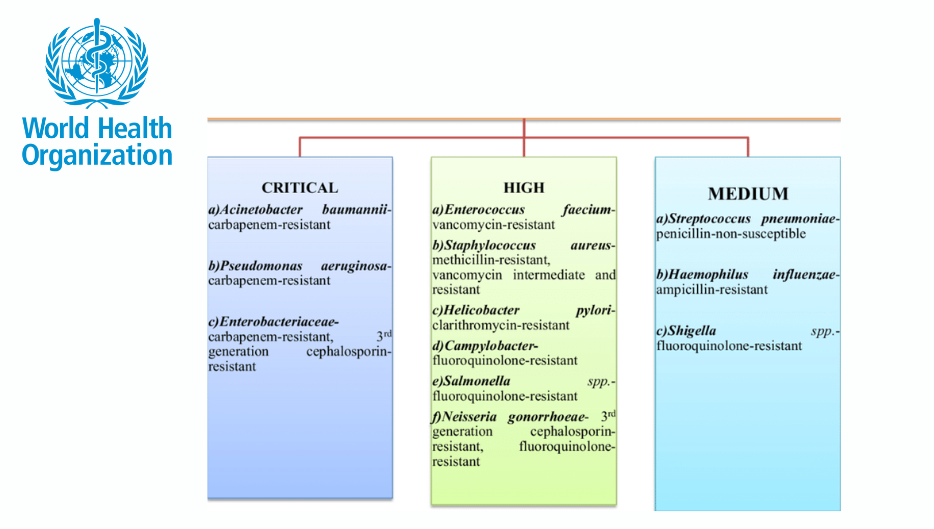
The revised BPPL includes three priority groups:
- Critical Priority: It includes germs like Acinetobacter baumannii, which is Gram-negative, and Mycobacterium tuberculosis, which is rifampicin-resistant. It is well known that these germs are hard to kill and can quickly spread resistance.
- High Priority: It has bacteria like Methicillin-resistant Staphylococcus aureus (MRSA) and Vancomycin-resistant Enterococcus faecium. In healthcare situations, these pathogens are very dangerous.
- Medium Priority: Pathogens like Group A and B Streptococci are in this medium-priority group. These pathogens still need a lot of attention to keep them from having general effects on health.
Updated Strategies and Your Role
The threat of AMR requires concerted efforts not just from healthcare providers but also from the public. Here’s what you can do to contribute:
- Antibiotic Stewardship: Use antibiotics only as prescribed and complete their full course. Avoid requesting antibiotics for viral infections such as the common cold.
- Hygiene Practices: Regularly wash hands, Maintain rigorous food hygiene, and Keep environments clean to prevent the spread of infections.
- Vaccination: Stay up-to-date with vaccinations to reduce the risk of bacterial infections and this indirectly combats AMR.
- Awareness and Advocacy: Educate yourself about AMR and advocate for public policies that encourage prudent antibiotic use and enhance infection control measures.
More About Antibiotic resistance
Antibiotic resistance, a big threat to the whole world, happens when bacteria change so they can avoid antibiotics. This makes it harder to treat common infections. Alexander Fleming, who found penicillin in 1928, worried about resistance from the start. Lack of methicillin Staphylococcus aureus (MRSA) was found only two years after methicillin was first used, in 1960. Soil bacteria are the main natural source of antibiotics, which shows that development has been going on for thousands of years. Some bacteria have genes that make them “pan-resistant,” which means they can’t be killed by any known drug. Resistance risks are greatly increased when used too much in crops. New laws aim to limit the use of antibiotics for non-essential purposes, which is very important for protecting future medical treatments. Researchers think that if things keep going the way they are, antibiotic-resistant bugs could kill 10 million people every year by 2050.
Month: Current Affairs - May, 2024
Category: International / World Current Affairs